September 7, 2024
The Duty Of Hormones In Female Urinary Health
Urinary Incontinence Medical Diagnosis And Treatment If left neglected, these skin disorders may result in push sores and ulcers, potentially causing additional infections. The exact prevalence of urinary incontinence is challenging to estimate. Component of the problem has remained in defining the degree, amount, and frequency of pee loss required to certify as pathologic, with varying meanings amongst research studies.
Just How Hormonal Agent Replacement Treatment Effects Urinary Incontinence
What hormonal agent stops pee?
make less pee in the evening. Takeaway: If progesterone degrees are rising throughout and after your cycle, and progesterone triggers your bladder to get a lot more frequently, it may create incontinence. Menstrual changes. There are numerous factors your monthly duration can alter, yet hormone inequality often plays a role.Hair problems.
The junction of cylindrical cobblestone coverage and columnar and improvement area moves a whole lot to the endocervical canal that produces issues in Pap examination and colposcopy. Incident or worsening of signs and symptoms focused on tension, urge, and mixedUI reported at standard and 1 year. Females stratified by standard UI were analyzedin the treatment groups to which they were originally randomized accordingto the intent-to-treat principle. Individuals with missing information on UI atbaseline or 1 year were left out from the analyses. Evaluations were performedusing SAS statistical software (variation 9.0, SAS Institute Inc, Cary, NC). The research study pills were likewise ceased if anynonstudy estrogen or progestin was started.
Diet Plan And Hydration: Their Effect On Urinary Incontinence Phases
Low estrogen can cause bladder signs and symptoms by thinning the tissue that lines the vaginal canal. This reduces the flexibility and toughness of the vaginal canal and bordering muscular tissues, decreasing muscle support for the bladder and related frameworks, such as the urethra. Nevertheless, not all people with low estrogen develop bladder problems. For instance, people who have actually previously given birth might have pelvic floor disorder.
- These questions can help your company figure out a pattern with your leakage, which commonly points to a details sort of incontinence.
- The specific feature and significance of these muscle mass are controversial.
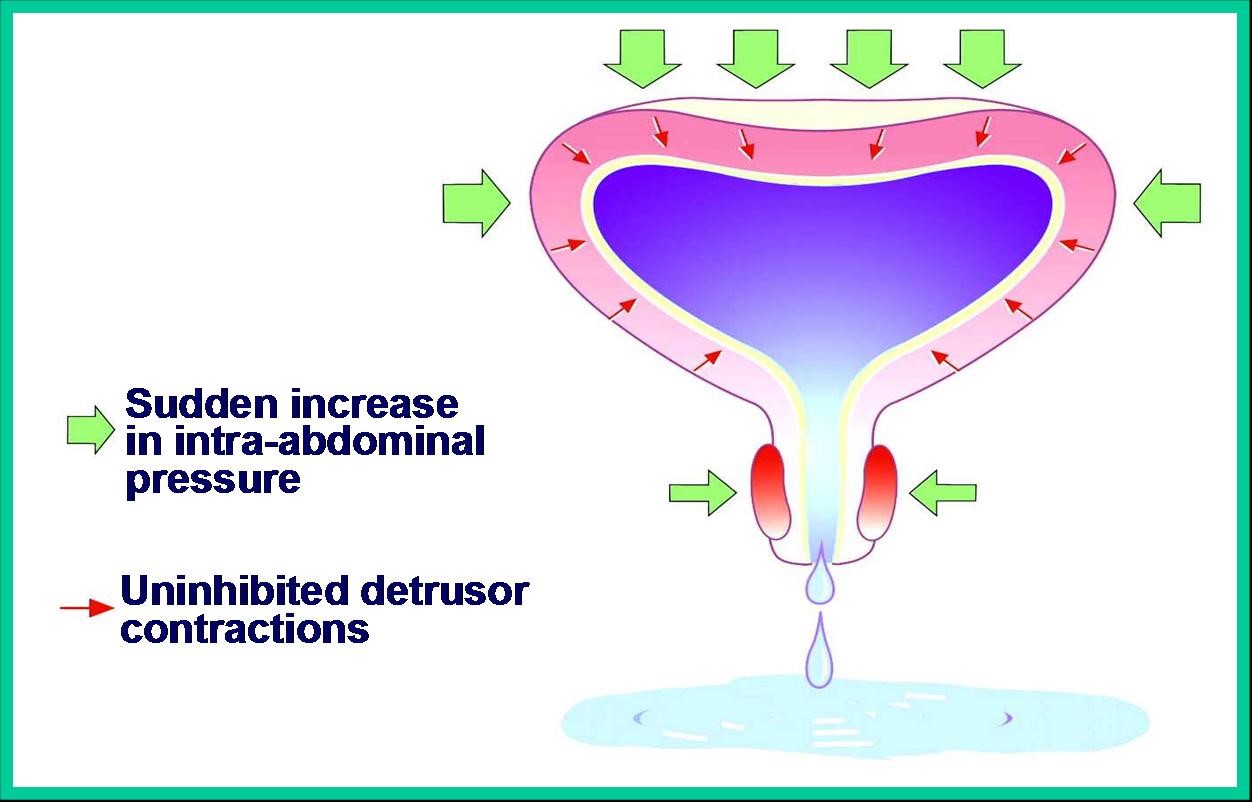
- The outcome can be a little leak of urine or a total loss of control.
- Study suggests that it does not raise the levels of oestrogen in the blood significantly.
- Any unusual neurologic indications should be pursued by a complete neurologic assessment.
It might additionally boost the amount you have the ability to urinate at one time. If genital dryness and urinary incontinence are your key signs and symptoms, topical estrogen therapy might be a great option for you. This treatment gives your body additional estrogen in the kind of creams or rings. As you age, your estrogen levels decline significantly-- especially throughout menopause. One of the most usual genetic disorders triggering incontinence consist of ectopic ureter( s), and relevant structural abnormalities (patent urachus, pseudohermaphrodites, and urethrorectal fistulae). Congenital malformations of the sacral spinal cord can likewise trigger neurologic disorder causing a flaccid, overdistended bladder with weak discharge resistance. Clients whose urinary incontinence is treated with catheterization additionally encounter threats. Both indwelling catheters and intermittent catheterization have a variety of prospective difficulties (see Treatment). Although data concerning urinary system incontinence in people of different races are sparse, reports are arising that race
Frequent urination might play an essential duty in the frequency and likelihood of coverage of incontinence. The duty of estrogen and progesterone and p53, in creating prolapse of pelvic organ and tension pee incontinence is reported in countless study studies [19] That based upon the subject of this short article, a number is discussed. Results of various research studies show that genital atrophy, uterine prolapse, cystocele, Rectocele, Ectropion, cervix ulcer and irritability in females boosts. The urethral syndrome, nocturnal enuresis, urinary system system infection is reported in 7% - 10% of postmenopausal women [20] In a study by Zhu and his colleagues, the level of estrogen receptor in tissues of Pelvic floor of patients with anxiety incontinence was reported substantially lower than the control group [22]