September 7, 2024
Monitoring Of Urinary System Incontinence In Postmenopausal Women: An Emas Clinical Overview
Remedies For Your Urinary System Incontinence: Melissa Grier, Md: Obgyn These take a trip up the tibial nerve to the sacral nerve plexus, which regulates the bladder. PTNS sessions are pain-free, last thirty minutes and are duplicated once a week for 12 weeks. As a result of this, imipramine may serve for nighttime incontinence. When used properly, topical estrogen therapy usually does not cause adverse effects.Kegel Workouts
Encouraging females with understanding regarding treatment choices, coping methods, and preventive measures can aid them take care of urinary system incontinence efficiently and live confidently. Reduced estrogen degrees during menopause can weaken the pelvic floor muscular tissues and the urethral sphincter, adding to urinary incontinence. The American University of Obstetricians and Gynecologists (ACOG) specifies that routine physical activity and maintaining a healthy and balanced weight are key consider preventing UI and enhancing bladder control. The ACOG also recommends pelvic flooring muscle mass workouts, also called Kegel workouts, to enhance the muscular tissues that sustain the bladder.Other Techniques To Dealing With Tension Urinary Incontinence
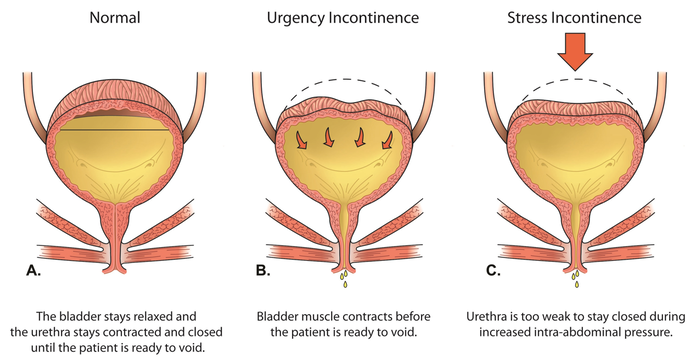
Make a consultation with a health care expert if you have problems regarding your bladder behaviors or leaks. At your visit, you'll have a physical exam and talk with your medical professional regarding your signs and symptoms. Aeroflow Urology recognizes managing urinary incontinence signs and symptoms can be hard at times, especially if you're also managing signs of menstrual cycle. Allow us do the help you concerning incontinence care by sending you totally free incontinence products on a monthly basis if you certify. It is the factor for your duration, pregnancy (if you determine that's right for you), and menopause. Modifications in the bladder and urethra throughout menopause can likewise add to urinary incontinence. The bladder muscular tissue can become less adaptable, causing a reduction in bladder capacity and a boosted frequency of urination. Furthermore, the urethra can come to be shorter and less elastic, making it harder to preserve continence. These anatomical changes can lead to a heightened sensitivity to bladder filling, triggering an urgent requirement to urinate even when the bladder is not full. The loss of estrogen can also lead to thinning of the urethral lining, more compromising its capacity to function efficiently and raising the probability of urinary incontinence. If you are overweight, even 5% weight management can enhance urinary seriousness substantially.Managing Urinary System Incontinence In Women: Services And Support
What is the most effective medicine for urinary incontinence?
TREATMENT OF IMPULSE INCONTINENCE
The anticholinergic representatives oxybutynin (Ditropan; Oxytrol) and tolterodine (Detrol) are made use of extensively to treat urge incontinence.
- This guide intends to debunk FEUCs, comparing them to typical methods and highlighting what you need to consider prior to making a choice.
- The physical stress of pregnancy and giving birth can in some cases cause medical therapies to fail.
- Additionally, liquid monitoring is essential; females need to intend to consume adequate water throughout the day while preventing extreme intake before bedtime to decrease nighttime peeing.
- According to a research study published in the Journal of American Urogynecologic Society, over 60% of adult females in the United States experience this embarrassing problem.
- You don't have to accept occasional bladder leak as another adverse effects of menopause or aging.
Social Links