September 7, 2024
Menopause And Urinary Incontinence
Monitoring Of Urinary Incontinence In Postmenopausal Females: An Emas Scientific Overview You may be described a medical professional that specializes in urinary system disorders (urologist) or a gynecologist with unique training in women bladder issues and urinary system function (urogynecologist). Your doctor may recommend that you do these workouts regularly to reinforce the muscles that aid manage peeing. Also referred to as Kegel workouts, these strategies are particularly effective for stress urinary incontinence but might also assist urge urinary incontinence. Estrogen depletion is among the indications of hormone discrepancy in females that is normally experienced during menopause. Among the most effective means to stay up to date with urinary system incontinence is with the use of grown-up diapers for ladies. Later on, in a subgroup of these individuals, myopathic adjustments might occur in the bladder that make the spread of abnormally created contractile signals more effective and harder to suppress willingly. These connective-tissue components create the passive supports to the urethra and bladder neck. During times of raised intra-abdominal stress, if these assistances are intact, they increase the helpful result of muscle closure of the pelvic floor. https://s3.us-east-2.amazonaws.com/5ghb9bmaj7etny/adipose-tissue/postpartum-recovery-answers-to-the-typical-questions-asked-by-br.html INNOVO's distinct Multipath ™ Innovation ensures optimal muscle involvement and effectiveness, providing targeted excitement to the pelvic floor muscular tissues without the demand for intrusive probes or hands-on intervention.Impulse Incontinence Pathophysiology
In addition, the individual relearns exactly how to regulate the bladder and strengthen the entailed muscles. Urinary bladder hypocontractility or bad lodging of pee during storage space may result in frequent leakage of tiny quantities of urine. Disorder may be brought on by urinary system infection, persistent inflammatory problems, neoplastic sores, external compression, and chronic partial electrical outlet blockage.Neurologic Reasons
It can also weaken your pelvic floor muscles, making it more challenging to keep in urine. Nonneurogenic urinary incontinence might be triggered by structural or useful conditions (e.g., ectopic ureters) affecting the storage space stage of micturition. Hormone-responsive urinary incontinence is likewise a common kind of nonneurogenic urinary system incontinence. In these patients (usually pet dogs), the detrusor reflex is typical; typical peeing actions, along with pee dribbling, occurs.Therapy For Reduced Estrogen Bladder Signs And Symptoms
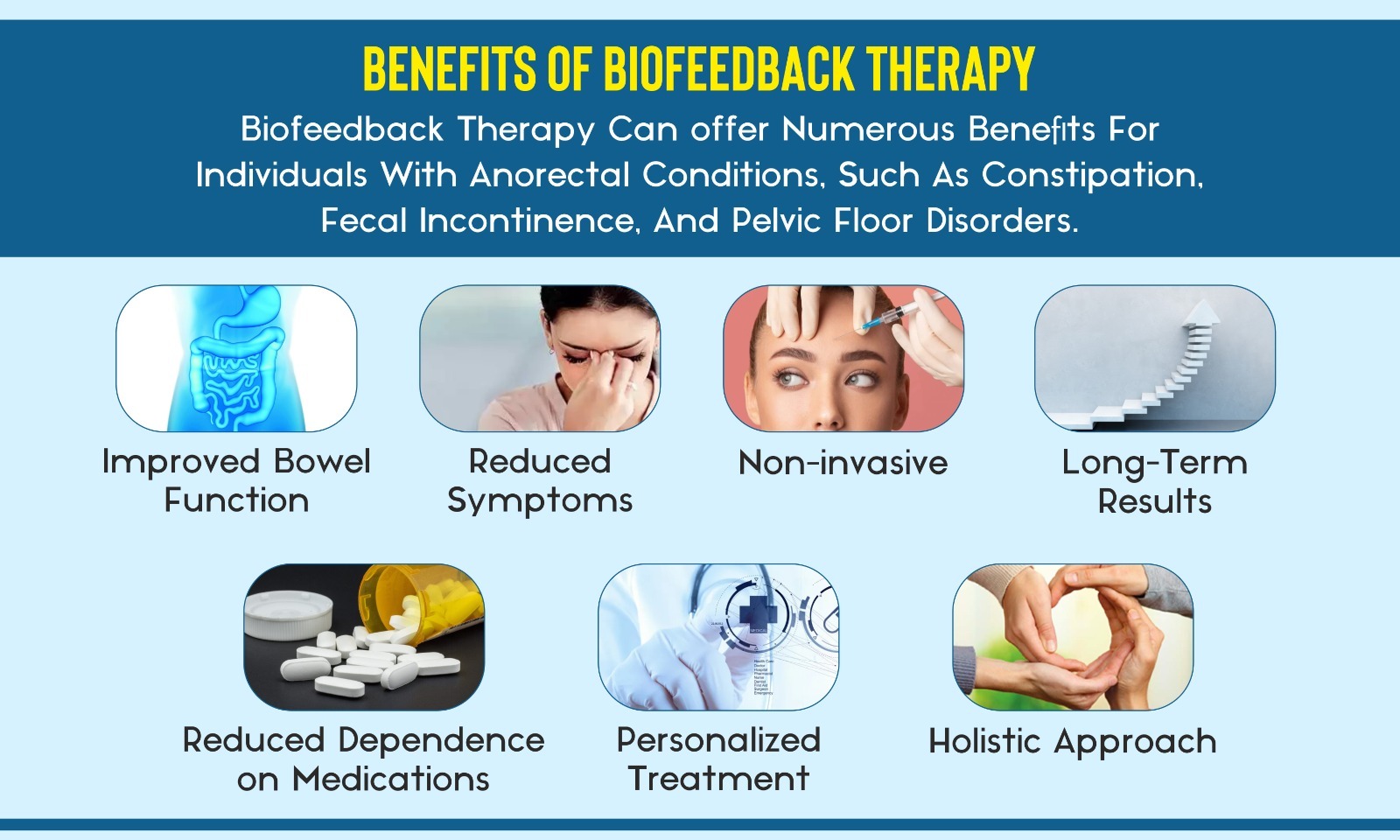
Subject estrogen products might also aid to tone your urethra and vaginal areas. Electrical treatments are applied directly over the pelvic floor muscles. Biofeedback to strengthen and collaborate the pelvic floor muscles. Psychophysiological feedback is coordinated with pelvic flooring (Kegel) workouts. Alpha-adrenergic agonists may be provided for the monitoring of urethral incompetence, alone or in mix with reproductive hormonal agents, where a synergistic impact is occasionally observed.- The psychosocial costs and morbidities are a lot more challenging to evaluate.
- Your healthcare service provider may recommend duplicating the shots one or two times a year.
- If various other methods for aiding stress urinary incontinence do not work, your physician might recommend surgical treatment.
- The most common genetic disorders causing incontinence include ectopic ureter( s), and relevant anatomic abnormalities (license urachus, pseudohermaphrodites, and urethrorectal fistulae).
How can bladder leakage be stopped?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and sleep issues.Digestive distress. Using low-dose, topical estrogen may aid. The drug comes in the type of a genital cream, ring or spot. The estrogen might aid recover the cells in the vagina and urinary system to ease some signs. Topical estrogen may not be safe for individuals with a history of breast cancer, uterine cancer cells or both. Summary. Bladder disorder is an usual challenge, particularly later in life and throughout times of major hormonal adjustment. Reduced estrogen bladder signs and symptoms can consist of incontinence, overactive bladder, and pain.
Social Links