September 7, 2024
Management Of Urinary System Incontinence In Postmenopausal Ladies: An Emas Scientific Overview
Anxiety Incontinence: Causes, Signs And Treatment Refined blockage and the impacts old on smooth muscle mass and the autonomic nervous system are 2 feasible factors. When the urethra is hypermobile, pressure transmission to the wall surfaces of the urethra might be lessened as it descends and revolves under the pubic bone. Intraurethral stress drops listed below bladder stress, leading to urine loss. Some hypothesize that under typical scenarios, any kind of increase in intra-abdominal stress is transferred just as to the bladder and proximal urethra. This is likely because of the retropubic place of the proximal and mid urethra within the sphere of intra-abdominal stress.What Causes Urinary Incontinence?
What hormone stops pee?
earn less pee at night. Takeaway: If progesterone levels are increasing throughout and after your cycle, and progesterone triggers your bladder to get much more often, it may create incontinence. Menstrual changes. There are many factors your month-to-month duration can transform, however hormonal inequality often plays a role.Hair concerns.
Reasons To Pick Laparoscopy Over Standard Treatment
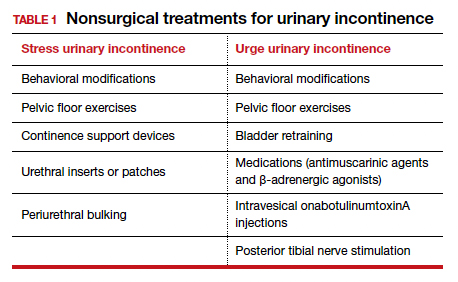
Throughout a lady's life, from adolescence to menopause, the delicate equilibrium of hormones manages a symphony of modifications that can affect urinary system continence and pelvic floor toughness. In some cases, there are modifications to your daily life that can in fact aid your urinary incontinence. These adjustments usually include workouts you can do to reinforce your pelvic flooring muscle mass, changes to your normal behaviors and an enhanced diet plan. Some individuals notice enhancements by making these modifications in your home and don't need additional therapy. Throughout this procedure, the posterior wall of the urethra shears off the former urethral wall to open the bladder neck when intrinsic sphincter deficiency is present. Useful urinary incontinence is the lack of ability to hold urine due to reasons other than neuro-urologic and lower urinary system disorder. Videourodynamic researches are reserved to examine complicated cases of anxiety urinary incontinence. Urethral inexperience typically results in periodic urinary incontinence, typically at remainder. Hormone treatment (estrogen) in postmenopausal females relieves urinary regularity which results in enhance in the toughness of muscles around the bladder. Althoughbasic scientific research in this area is restricted, a current placebo-controlled, randomizedclinical trial of estrogen alone sheds light on this problem. Urethral closureis based on the incorporated action of the suburethral vaginal wall, thepubourethral ligaments, the pubococcygeus muscles, and the paraurethral connectivetissues. As you age, the muscular tissues that sustain your pelvic body organs can weaken. This implies that your bladder and urethra have less assistance-- usually bring about urine leakage. Many women experience premenstrual disorder (PMS) about 1-2 weeks before hemorrhaging starts. An all natural approach that utilizes medicine, way of life adjustments, physical therapy, or various other interventions may help reduce them or help somebody handle them. Many people believe that it's something that simply supports aging and is an inevitable problem. If you discover that urinary incontinence is troubling your daily activities and causing you to lose out on things you usually take pleasure in, talk with your doctor.- Nerve damage can interrupt signals from your bladder to your mind so you don't experience the urge to urinate.
- The pubourethral ligaments likewise suspend the middle part of the urethra to the back of the pubic bone.
- Estrogen is released in your body before and during ovulation, and thickens the uterine cellular lining to prepare the womb all set for pregnancy.
- Vasoactive intestinal tract peptide, a smooth muscle mass relaxant, is lowered markedly in the bladders of patients with detrusor overactivity.
- Throughout sacral nerve stimulation, an operatively implanted tool provides electrical impulses to the nerves that regulate bladder task.
Social Links