September 7, 2024
Stress Urinary Incontinence: Reasons, Symptoms And Therapy
Stress Urinary Incontinence: Reasons, Signs And Treatment Comparing volunteer and spontaneous peeing is essential to the diagnostic strategy. Three sorts of lesion of disintegration, ectropion and cervical lesions in post-me- nopause is seen much more. Endocervix glandular cells task throughout menopause and ultimately the amount of mucin lowers that this creates to vaginal dryness that occurs as a primary issue in postmenopausal women. Mild electric stimulation can be effective for stress and anxiety urinary incontinence and urge incontinence, however you may require multiple treatments over numerous months. Obstructive conditions should be handled as rapidly as feasible. Urinary system system infection should be treated with ideal clinical therapy. Ectopic ureters and other congenital anomalies can be surgically fixed; the clinician needs to know that practical problems of urinary bladder storage or urethral competence might accompany this flaw.Urinary Problems
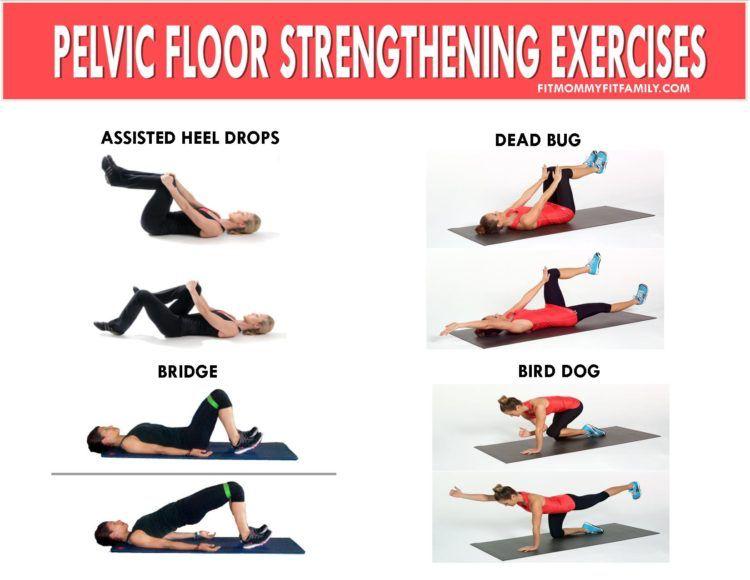
As a result of the setting and feature of steroids in the urinary system system, using changed hormonal agent treatment in menopause has long drawn in the attention of scientists and suppliers of health care in this area. In women without urethral hypermobility, the urethra is maintained during stress and anxiety by 3 related devices. One device is response, or volunteer, closure of the pelvic flooring. Contraction of the levator rectum facility elevates the proximal urethra and bladder neck, tightens intact connective tissue sustains, and elevates the perineal body, which might work as a urethral backstop. If you're experiencing urinary incontinence throughout your duration or your cycle, it can alter your quality of life.What Creates Urinary System Incontinence?
In 1989, the National Institutes of Wellness Consensus Growth Conference approximated the annual expense of urinary incontinence in the United States to be $12.4 billion. Real expenses can be difficult to approximate because lots of individuals do not come to the interest of clinical experts. Urinary system incontinence needs to not be thought of as an illness, because no certain etiology exists; most specific cases are likely multifactorial in nature. The etiologies of urinary incontinence are diverse and, oftentimes, incompletely understood. It is necessary to inform your doctor or nurse if you are having troubles. Find out if you qualify to get incontinence products free through your insurance at the end of the page. An individual must talk with a doctor if they have any kind of concerns they might have reduced estrogen or if they are experiencing bladder signs. Low estrogen can also affect people outside of menopause, specifically after delivering or during breastfeeding. As lots of as 15% of premenopausal females might have GSM-like signs therefore. However, they can likewise go down during various other stages of life, such as after giving birth or while breastfeeding.- Occurrence or worsening of symptoms concentrated on stress and anxiety, impulse, and mixedUI reported at baseline and 1 year.
- People with incontinence frequently deal with this condition for 6-9 years before looking for clinical therapy.
- The hollow member by sustaining muscles is placed in a best location and if for any kind of reason the sustaining muscles lose the ability, bladder displaced from its location and creates problems for the person.
- Cauda equina disorder can create in clients with a huge centrally extending disk.
What hormonal agent keeps you from peeing?
Social Links