September 14, 2024
Mixed Incontinence: What Are Your Therapy Alternatives? National Organization For Continence
Urinary Incontinence In Ladies: Kinds, Therapies, And Overview Genital mesh surgical procedure is where a strip of synthetic mesh is inserted behind television that carries pee out of your body (urethra) to sustain it. If you have a vaginal canal, a colposuspension can aid protect against spontaneous leakages from tension urinary incontinence. For transgender men (designated woman at birth), the procedure causes lowered estrogen levels.- You can experience UI throughout your life, yet most episodes are the result of pressure or anxiety on the muscles that aid you hold or pass pee.
- Sling surgical treatment entails making a cut in your reduced stomach (abdominal area) and vaginal canal so a sling can be put around the neck of the bladder to sustain it and avoid pee leaking.
- The goal of this medical overview is to provide an evidence-based technique to the administration of urinary incontinence in postmenopausal women.
- Injections of Botox into the bladder muscular tissue might profit people who have an over active bladder or urge urinary incontinence.
Urinary Incontinence In Women: Obstacles And Remedies
Incontinence can occur when the bladder muscles unexpectedly tighten up and the sphincter muscle mass are not solid enough to pinch the urethra shut. This causes an unexpected, strong desire to pee that you might not be able to regulate. Stress caused by chuckling, sneezing, or exercising can cause you to leakage urine. Urinary system incontinence may likewise happen if there is a trouble with the nerves that regulate the bladder muscular tissues and urethra.Urinary System Diversion
Progesterone additionally tells your body to let go of all the liquid it held onto throughout your period, including urine. When this happens, you might really feel the demand to nullify much more regularly, which is the primary signs and symptom of OAB. The research additionally reported that ladies were experiencing noticeably boosted task in their detrusor muscular tissue complying with ovulation. The change of progesterone and estrogen is why you experience signs during your cycle and while on your period. The majority of females experience premenstrual disorder (PMS) concerning 1-2 weeks prior to hemorrhaging begins. Progesterone is a hormonal agent launched by your ovaries throughout your menstrual cycle. Much more recently, clinical reports have shown up that issue the change in the lifestyle and sex-related function of females undertaking surgery in SUI. The outcomes of the carried out research plainly show that the high quality of females's life after procedures improves dramatically. On top of that, their wellness, self-esteem and confidence are enhanced. Oftentimes, medications can function effectively to return regular function to the bladder. Your carrier will meticulously pick a medicine that matches your certain needs. Frequently, your service provider will certainly begin you on a reduced dosage of the medication and after that boost it slowly.What sort of hormone treatment can treat urinary incontinence?
Numerous researches have shown that oestrogen replacement can boost, or even cure, urinary anxiety and prompt urinary incontinence.
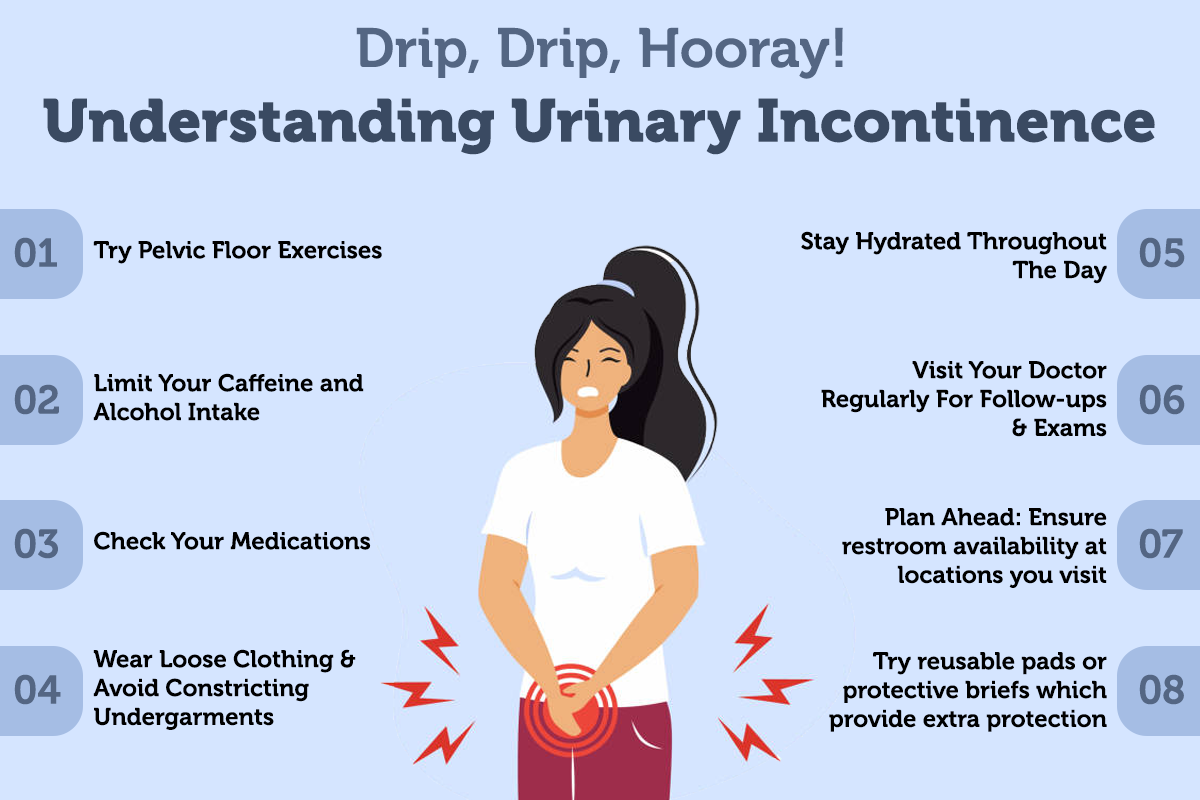
What To Do Regarding Urinary Incontinence
Well, while there isn't much urodynamic research to Helpful site describe the relationship in between menstruations and urinary system incontinence, there is a frequency of incontinence symptoms during females's durations. If you have menopause in addition to one of the list below problems, your risk of developing UI rises. You do not need to accept periodic bladder leak as an additional side effect of menopause or aging. In many cases, there are points you can do to stop and also avoid urinary incontinence. Bladder training can be helpful for decreasing leakages of UUI by adhering to a set washroom routine. The primary objective of carrying out a bladder training routine is to increase the time span between shower room journeys. Coping methods and support group play a critical function in managing the emotional aspects of incontinence. Women can take advantage of establishing a network of good friends, family members, or support groups who understand their experiences and can supply encouragement. Participating in open discussions concerning urinary incontinence can help reduce feelings of isolation and shame, promoting a sense of community and shared understanding. These strategies can dramatically improve comfort and self-confidence for females experiencing incontinence throughout this transitional phase. This Cochrane Testimonial, conducted by the Cochrane Incontinence Team, evaluated 34 trials entailing over 19,000 ladies with urinary system incontinence. The Simon Structure site material is for educational functions just and does not change advice from healthcare professionals. In some cases, urinary incontinence can indicate a a lot more serious underlying problem or neurological issue. Overflow urinary incontinence happens when a bladder does not completely vacant. If you struggle with overflow urinary incontinence you may experience normal, continuous pee dribble throughout the day. You can also get pads or protective undergarments while you take various other actions to deal with urinary system incontinence. These are marketed in several shops that additionally market feminine health products like tampons and pads. Be patient as you work with your doctor or registered nurse on a treatment plan. Acupuncture may aid by promoting relaxation and enhancing pelvic flooring muscle function, potentially minimizing signs of urinary incontinence. These choices can be especially appealing for women looking for non-surgical interventions. Analysis examinations, consisting of urinalysis, pee culture, and blood tests, play an important role in ruling out underlying medical conditions that may contribute to urinary system incontinence. It can be awkward to discuss restroom practices with your healthcare provider. This embarrassment shouldn't stop you from treating incontinence, though. Usually, your healthcare provider can assist figure out the cause of your bladder control issue and assistance make it better. Speak with your doctor regarding the very best methods to deal with incontinence to ensure that you can lead a full and active life without stressing over leak.Social Links