September 8, 2024
The Concealed Health Influence Of Urinary System Incontinence What You Require To Recognize
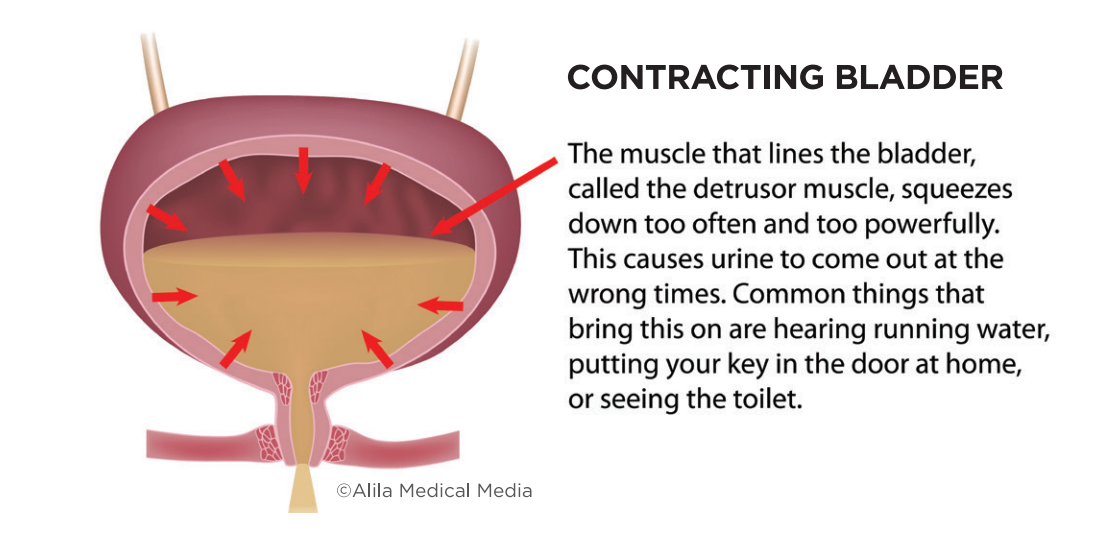
The Emotional Effect Of Impulse Urinary Incontinence In men with BPH, a bigger Overactive Bladder (OAB) prostate is kept in mind on physical examination. In many cases, even more examination might be required to eliminate prostate cancer or other obstructive problems.301 The professional discussion of OFI is characterized by reduced urinary system tract signs and symptoms (LUTS). This spectrum of signs arises from compression of the urethra, which consequently results in an unsteady detrusor muscular tissue or to bladder distention and hypertrophy triggered by the client's chronic failure to completely clear the bladder.- Urinary system urinary incontinence usually is the primary factor for institutionalization of senior individuals.
- Stress And Anxiety Reduction Strategies Stress can exacerbate urinary system incontinence.
- There is limited capability of a healthcare provider to anticipate the lifestyle of an individual incontinent woman.
- Beginning a conversation is the primary step to recognizing the medical and way of life choices that can help improve the signs of OAB.
What Are Psychological Factors For Moistening?
How can I quit urinary incontinence quickly?
Pelvic flooring muscle mass workouts
These exercises, called Kegels, reinforce the abdominal muscles that aid regulate peeing. Photo that you''re trying to quit the circulation or urine. If you''re making use of the best muscular tissues you''ll feel a pulling feeling. Draw in your pelvic muscles and hold for a matter of three.
Urinary System Incontinence In Older Females: That Is At Risk?
Necessity without actual urge-related pee loss also is an usual issue of people with stress and anxiety urinary incontinence. Less than 50% of the females in this evaluation reported looking for therapy from a medical professional regardless of having medically constant incontinence. These outcomes recommend that wellness system accessibility variables alone can not make up the reduced rates of treatment seeking for urinary incontinence that have been observed in the community. Additionally, identifying the sorts of beliefs regarding UI can discuss private differences in help-seeking habits and relevant end results (such as coping approaches embraced and conformity with medical programs) (Minassian et al., 2012; Bascur-Castillo et al., 2019). Literary works papers that only 25% of damaged females look for treatment, and less than half receive therapy (Minassian et al., 2012). In either situation, urethral sphincter feature is impaired, resulting in urine loss at lower than typical stomach pressures. This research exposes a number of vital fads in the quality-of-life effect and treatment of urinary system incontinence in ethnically diverse ladies in the USA. In this populace of ladies with a minimum of once a week continuous urinary incontinence, quality-of-life effect differed dramatically depending on factors related to the timing and setting of signs and symptoms. Such effects include new-onset lower urinary system tract dysfunction and prolapse. Such modifications might be minor, such as a change in the instructions or pressure of the urinary system stream. Alternatively, major modifications might happen, including a requirement to utilize self-catheterization for an extended postoperative period. It is also well known that pelvic floor conditions seldom happen alone.Social Links